Training today, impacting research tomorrow
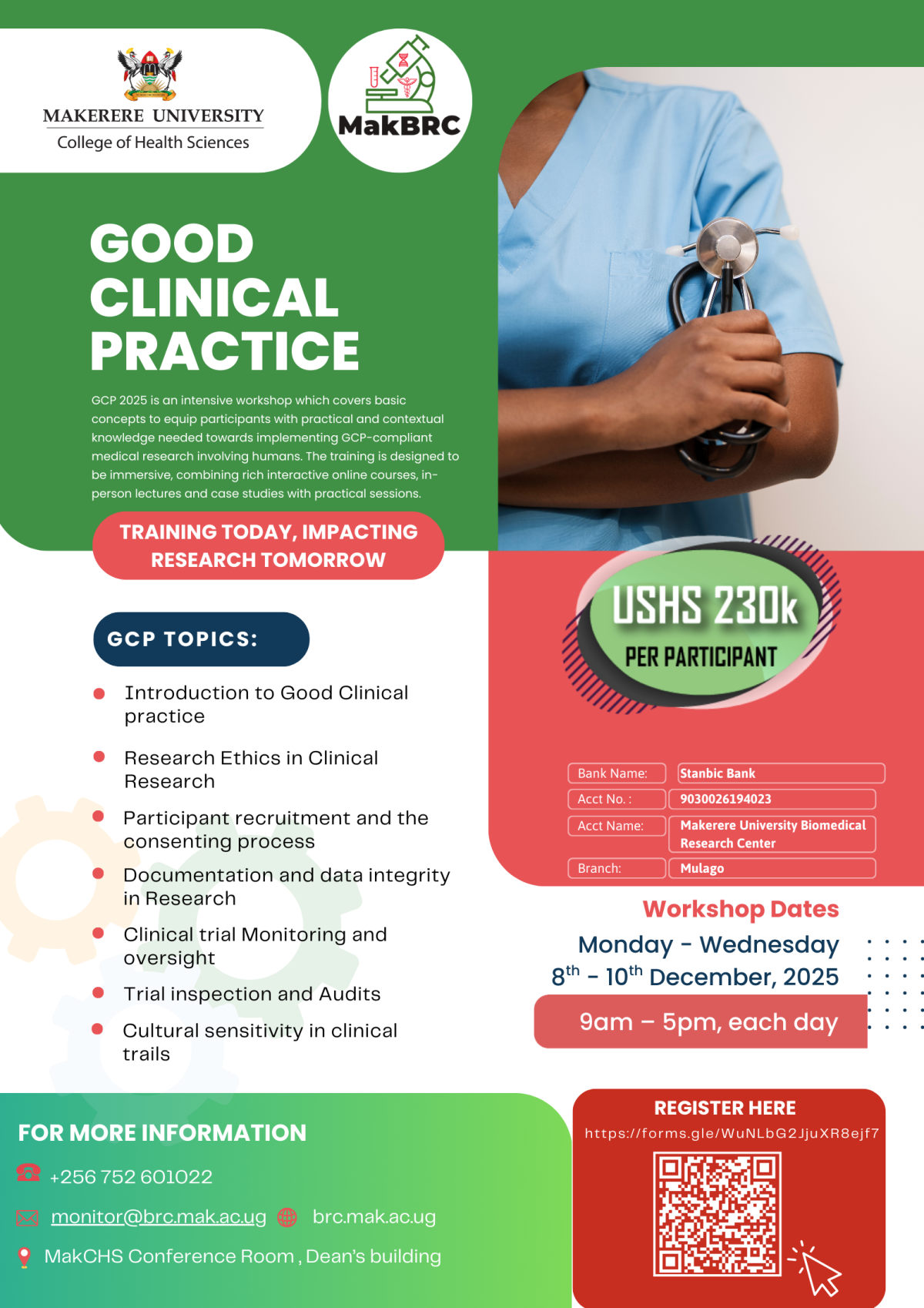
Makerere University College of Health Sciences, through the Biomedical Research Centre (MakBRC), invites you to the Good Clinical Practice (GCP) 2025 Workshop.
This intensive training covers the essential concepts of GCP, equipping participants with both practical and contextual knowledge needed to implement GCP-compliant medical research involving humans. The workshop combines interactive online modules, in-person lectures, case studies, and practical sessions.
Key Topics
-
Introduction to Good Clinical Practice
-
Research Ethics in Clinical Research
-
Participant recruitment and the consenting process
-
Documentation and data integrity in research
-
Clinical trial monitoring and oversight
-
Trial inspection and audits
-
Cultural sensitivity in clinical trials
Workshop Details
📅 Dates: Monday – Wednesday, 08th – 10th December 2025
🕘 Time: 9:00 am – 5:00 pm (daily)
📍 Venue: MakCHS Conference Room, Dean’s Building.
Fee: UGX 230,000 per participant
Registration
Register online here: Click to Register
Payment Details
-
Bank Name: Stanbic Bank
-
Account Number: 9030026194023
-
Account Name: Makerere University Biomedical Research Centre
-
Branch: Mulago